Our Impact
The NIHR Manchester BRC is the beating heart of translational research across Greater Manchester, Lancashire and South Cumbria, transforming scientific breakthroughs into diagnostic tests and life-saving treatments for patients.
Awarded £64.1 million for 2022-28, Manchester BRC brings together world-leading researchers based at The University of Manchester and six of the country’s foremost NHS Trusts, with a vision to drive forward health improvements.
Our year: 2024-25
We are delighted to share highlights from our 2024-25 Annual Report to demonstrate the impact Manchester BRC has made across our diverse communities.
Here we focus on some of our key outcomes, outputs and progress to date showcasing how we are delivering lasting change for all through creative, inclusive, and proactive research that identifies and bridges gaps between new discoveries and individualised care.
Professor Anne Barton, Director of Manchester BRC, introduces our key achievements from 2024-25

Read a summary of our key achievements from from April 2024 to March 2025. (opens in new window)
In this summary, we look back at some of the highlights from our 2024-25 Annual Report to showcase the positive impact we made across our diverse communities. Covering activity from 1 April 2024 to 31 March 2025, we demonstrate how we are delivering lasting change for all through creative, inclusive, and proactive research.
Read the Annual Report Summary 2024/25 in an accessible HTML format.
Who we are
The NIHR Manchester BRC is made up of:

We believe in Team Research – collaborating across different fields and professions to deliver cross-disciplinary science, from clinicians to engineers and project managers to health economists. We know research is enhanced through the collective input, strengths and expertise of many different people working together in a team, which is why we support a Team Research approach.
To find out more about our people, please visit our Leadership Team and Core Team pages.
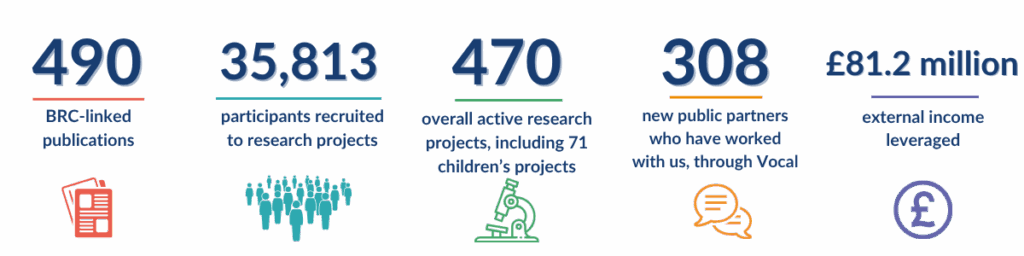
This year we had…
What our research has changed
Read our impact case studies from 2024/25 below.
NIHR Manchester BRC research will impact every new asthma diagnosis made in the UK and beyond. This means more people will be getting the right diagnosis, and fewer people will be taking the wrong treatment for their symptoms.
Why is this research important?
Asthma affects up to 7 million people in the UK, with 200,000 people diagnosed with the disease each year. This costs the UK economy an estimated £21 billion a year.
Around 1 in 3 of these people may not have asthma which could lead to inappropriate and ineffective treatment. This is likely due to poor evidence that underpins diagnostic guidelines, and lack of access to tests in primary care.
What did we do?
Researchers from our Respiratory Medicine Theme set up the Rapid Access Diagnostics for Asthma (RADicA) study, which aims to develop new and better breathing tests to diagnose asthma.
Since 2017, we have recruited more than 400 adults and children with suspected asthma. The results of the RADicA study show that current guidelines perform poorly, misdiagnosing asthma in at least 1 in 6 people.
We gave the National Institute for Health and Care Excellence (NICE) direct access to study data. This allowed them to produce new UK-wide joint guidance for the diagnosis and management of chronic asthma in adults, young people and children.
The data helped make the NICE pathway efficient (using tests which give the most unique information), clinically effective (against the gold standard in RADicA), and cost-effective.
The new guideline, underpinned by RADicA data, will impact every new diagnosis made in the UK and beyond. It will result in more people getting the correct diagnosis, and fewer people taking the wrong treatment.
We have brought in additional funding from NIHR, charity and industry and are supported by the NIHR Manchester Clinical Research Facility and NIHR HealthTech Research Centre for Emergency and Acute Care.
Our study is also providing a platform for small and medium-sized enterprises (SMEs) to test new diagnostics.
What will we do next?
We are exploring working with the NIHR Applied Research Collaboration-Greater Manchester to develop a project to measure and improve uptake of the new guidance and assess associated outcomes.
NIHR Manchester BRC research has improved diagnosis, changed service delivery nationally and internationally and is at the forefront of developing and delivering gene-based treatments for people with inherited eye diseases, which lead to vision loss and blindness.
Why is this research important?
Inherited eye diseases (IEDs) lead to vision loss and blindness, often due to changes in genes responsible for maintaining healthy sight.
These conditions have considerable costs on the individuals affected, the NHS and society.
Before 2012, genetic testing was only available to a small number of families with IEDs. This left many affected families waiting years for a precise diagnosis, with limited treatment options.
What did we do?
To improve care and outcomes for people with IED, Professor Graeme Black, Next Generation Phenotyping and Diagnostics (NGPD) Co-Theme Lead at Manchester BRC, collaborated with Manchester Centre for Genomic Medicine, Manchester Academic Health Science Centre (MAHSC) and the NIHR Manchester Clinical Research Facility (CRF) to develop, and introduce genomic tests, driving the development of novel treatments.
This research has led to:
1. Improved patient outcomes by identifying disease processes in the human eye
One of the largest global IED cohorts of more than 8,000 people has been assembled to study eye diseases. Over the last 25 years, analysis has led to the discovery of over 35 genes that cause disease and over 100 genetic tests, listed in the National Centre for Biotechnology Information Genetic Testing Registry.
Manchester BRC continues to study this cohort and has recently introduced a new imaging technique in clinic because of this, called adaptive optics.
2. Changes in service delivery nationally and internationally
This work led to development and introduction of new ‘Next Generation Sequencing-based’ tests (DNA sequencing). Most recently, the genes responsible for albinism have been identified through the work of Manchester BRC researchers.
This work has also had international impact. The NGPD Theme:
- Led on drafting European guidelines for genetic testing for rare eye diseases
- Led work to ensure clinical information was coded in a standardised way cross countries.
- Were the sole ophthalmologists “instrumental in the design and structure” of DECIPHER, a web-based tool that captures clinical data in a standardised way. It currently shares more than 36,000 rare disease patient records from more than 250 clinical genetic centres worldwide.
3. The development of a gene therapy centre for eye diseases in the North of England
Manchester BRC, The University of Manchester (UoM) and Manchester CRF are at the forefront of developing and delivering gene-based treatments for IEDs.
In 2020, the team established the first ophthalmic gene therapy centre in the North of England, delivering gene-based treatments as standard NHS care. With healthcare scientists and health economists, the NGPD Theme is currently working to develop evidence to support future gene therapy approvals.
Patients have benefitted significantly because of this research. Retinal disease diagnostic rates have increased from less than 15% (pre-2012) to around 60-80% (2020-2024).
What will we do next?
The NGPD Theme will continue to support this work by:
- Collaborating with the Next Generation Therapeutics Theme health economists to advance implementation science (methods and strategies to promote uptake of evidence-based interventions into routine practice). This is a project in collaboration with industry partner Janssen.
- Building on cross-Cluster relation with the Rare Conditions Theme, NGPD aims to use integrative approaches to enhance the interpretation of whole genome sequencing data.
- Catalysing the development of new therapies through the introduction of advanced ophthalmic imaging technologies to mainstream clinical services, and the development of next-generation ophthalmic imaging devices (in collaboration with Manchester University NHS Foundation Trust Clinical Imaging and UoM Engineering and Optometry Departments).
- Combining, AI, genomics and ophthalmic imaging to predict risk of ophthalmic and neurodegenerative disorders (in collaboration with the Pankhurst Institute).
NIHR Manchester BRC research has helped make bladder cancer care more effective, fairer, and more accessible in the UK and in some countries around the world. Their evidence for a shorter radiotherapy schedule changed the approach of all cancer treatment centres in the UK as well as major international guidelines.
Why is this research important?
Bladder cancer is the 11th most common type of cancer in the UK. For people with advanced bladder cancer, survival chances are low – more than half die within 5 years of being diagnosed.
Treatment usually involves either removing the bladder through surgery (called a radical cystectomy) or having radiotherapy. Both treatments are similarly good at stopping the cancer from coming back. Patients often also receive chemotherapy before the main treatment to improve results. Surgery is a big operation that needs the patient to be in good health and takes time to recover from. Radiotherapy is less invasive and lets patients keep their bladders.
There are two common ways of giving radiotherapy for advanced bladder cancer:
- 64 Gy (dose of radiation) given in 32 sessions over 6.5 weeks, or
- 55 Gy given in 20 sessions over 4 weeks (a shorter, more intense course called “hypofractionated”).
This study aimed to see if the shorter, 4-week schedule works just as well and is just as safe as the longer, 6.5-week schedule.
What did we do?
During Manchester BRC 2017-2022, a comprehensive analysis of two major UK trials combining individual data from over 800 patients showed that a shorter course of radiotherapy is more effective and just as safe as the traditional longer schedule for treating locally advanced bladder cancer.
Bladder cancer grows quickly, which makes the length of radiotherapy treatment very important. This analysis found that the shorter 4-week schedule (55 Gy in 20 sessions) is not only just as good as the longer 6.5-week one, but even better at controlling the cancer in the bladder and surrounding area. In fact, it reduces the chance of the cancer coming back in about 1 in 3 patients.
Now, during Manchester BRC 2022-28, the evidence from Cancer Advanced Radiotherapy Theme researchers is influencing some international clinical guidelines, helping drive smarter, more sustainable cancer care across the globe.
The two major studies analysed (BCON, led by The University of Manchester and BC2001, led by The Institute of Cancer Research, London) found that combining radiotherapy with other treatments – like chemotherapy or methods to increase oxygen in tumours – can help patients live longer. Both studies used the two radiotherapy schedules mentioned above, but until now, no one had compared them directly.
Because of this evidence, the shorter radiotherapy schedule is now the standard treatment for preserving the bladder in patients with advanced bladder cancer – not just in the UK. All cancer treatment centres in the UK now follow this approach, and it’s also supported by major European and US guidelines.
This approach, known as hypofractionated radiotherapy, reduces pressure on NHS radiotherapy services while maintaining excellent patient outcomes.
Shorter treatment also has practical benefits. It means fewer hospital trips for patients, less disruption to daily life, and costs less for the healthcare system.
The research was done in partnership with the NIHR Biomedical Research Centre at The Royal Marsden and The Institute of Cancer Research.
What will we do next?
If this is implemented internationally it is a strong example of how data-driven policy can deliver both better care and better value.
This new way of giving treatment has also helped countries with fewer healthcare resources. For example, India now uses the shorter schedule of 55 Gy in 20 sessions. In countries like Uganda and Kenya, there may only be one radiotherapy centre for the whole country. By reducing the number of hospital visits needed, more patients can get treated, which makes a big difference in places where access to care is limited.
An NIHR Manchester BRC Patient and Public Involvement, Engagement and Participation (PPIEP) programme engaged people with laboratory research through a co-produced campaign which included filmmaking, creative workshops, events, blogs and social media content.
Why is this important?
Laboratory research is a crucial aspect of health research and helps to improve the lives of people affected by conditions like asthma, arthritis and cancer. Public awareness and involvement is often limited.
What did we do?
Vocal, community organisations from the Black & Asian Research Advisory Group (BRAG), young people’s research advisory group Voice Up and 5 people from Greater Manchester, Manchester BRC and Manchester CRF co-developed and co-produced the Let’s Talk Labs campaign to raise awareness of laboratory research and how it makes a difference to people.
Let’s Talk Labs:
- Focused on community perspectives and questions about research.
- Trained and mentored 5 participants to develop their own ideas and produce their own films.
- Enabled participants and community groups to identify the best ways to engage their communities in this topic.
The programme delivered:
- Training and mentorship in filmmaking to people from diverse backgrounds.
- Visits to laboratories and collaboration between filmmakers and researchers.
- Creative workshops and events which brought community members and researchers together including:
- A Voice Up workshop exploring laboratory research and career pathways.
- Cancer researchers discussing their work and cancer risk with Black African women at a unique Dance & Learn session.
- 5 films produced by community members;
- ‘How does lab research into breast cancer benefit my community?’
- ‘How do clinical trials work?’
- ‘How does laboratory research help people like me?’
- ‘How does laboratory research help people with asthma?’
- ‘Young people must have a say in research’
- 8 accessible blogs by researchers and research staff, highlighting their work and the difference that it makes to people.
- A 2-week social media campaign delivered with community partners.
All of the participants said they were likely to get involved in similar activities and to encourage others to take part in similar activities; 6 out of 7 reported that they would take part in research.
One person commented: “As a direct result of this project I am now taking part in a research project on diabetes in Black African/Caribbean society.”
Participants in the project reported that their ideas about lab-based research had changed: “Before I joined the project, I had quite a narrow view of laboratory research I thought it was more just in the lab, restricted to maybe a person in a white lab coat, but since joining the project, I’ve realised that it’s actually a much broader and bigger picture.”
A researcher noted: “This brings to life the message about doing research with people not to people.”
What will we do next?
- Identify more opportunities for participants to continue to be involved in our work.
- Continue to work in partnership with the community organisations to develop inclusive communications and engage audiences in research.
- Use the content created to promote research involvement, participation and laboratory research.
Our connections
Manchester BRC has long-standing experience of delivering collaborative commercial work with industry partners. Key commercial partnerships support our goal of improving people’s health through experimental research.
This year…

The NIHR Manchester BRC connects the very best pharmaceutical, diagnostics, digital technology and medical device organisations with our world-leading academics and clinicians to work together on the latest translational research. We prioritise co-development and collaboration with the commercial sector to enable wider adoption and impacts from our research.
We continue to strengthen our relationships with international companies, enhancing our reputation as a leading centre of globally competitive research.
Small and medium-sized enterprises (SMEs) are at the heart of innovation. Our partnerships with SMEs can provide the evidence base needed to turn novel ideas into clinical answers and look at ways they can be implemented into the NHS.
Visit our Innovation and Partnerships pages to find out how you can work with us.
Shining a spotlight on our research

Watch our Spotlight On films to find out more:
- Cancer
- Inflammation
- Under-Researched Conditions
- Advanced Diagnostics and Therapeutics Catalyst
- Innovation and Partnerships
Visit our news page and research theme pages where you can find our latest updates.
Read our mature impact case studies to see how we have made a difference
The success of Manchester BRC is based on the lasting impact we make to improve people’s lives across our diverse communities. Find out how we transformed scientific breakthroughs into diagnostic tests and life-saving treatments, delivering wide-ranging benefits to the health and care system.