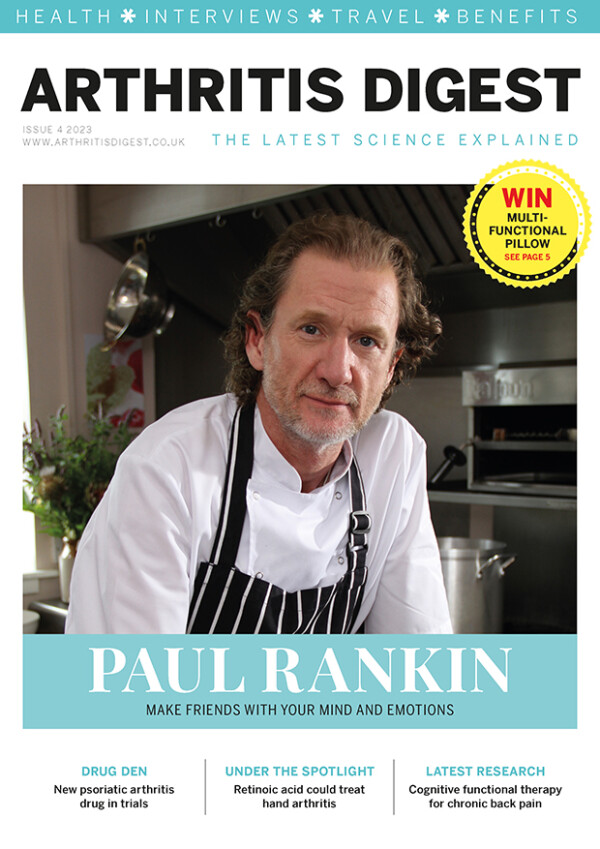
The opioid pendulum: Balancing the risks and benefits – Dr Meghna Jani speaks to Arthritis Digest
Arthritis Digest is a magazine for people with arthritis that highlights the latest relevant research and reviews topical issues. Continuing regular contributions from our researchers, Dr Meghna Jani discusses balancing the risks and benefits of using opioids to treat pain for people with musculoskeletal conditions.
Dr Jani is Training and Capacity Building Lead for the Rheumatic and Musculoskeletal Diseases Theme at NIHR Manchester Biomedical Research Centre, NIHR Clinician Scientist and Senior Lecturer at The University of Manchester and Honorary Consultant Rheumatologist at Salford Royal Hospital.
As a rheumatologist and clinical academic, she is interested in using digital data, especially from electronic health records, to evaluate the safety of medicines and improve personalised treatment for patients.
Musculoskeletal conditions are one of the most common reasons for prescribing opioid drugs such as codeine, tramadol, oxycodone and morphine. Whether it is knee pain, back pain, rheumatoid arthritis or fibromyalgia, it is likely that most of us know someone who has been on these pain medications.
Opioids are a broad group of drugs that act on areas of the brain and spinal cord to interfere with the transmission of pain signals. But what makes them effective for treating pain, at higher doses can also make them dangerous.
Opioid use and its related harmful effects have reached epidemic proportions in the US and Canada, with rising trends in the UK and other countries. However, there are limited options for pain relief and these drugs can be effective in the short-term.

Considered to be some of the strongest pain medicines available, opioids are used to treat pain after surgery, severe injury and cancer. Therefore, depriving everyone of opioids is not a solution. Balancing the benefit and harms and making informed decisions based on the scientific evidence is crucial, but how do we do this?
Current challenges
The opioid epidemic in North America has been one of the most high-profile public scandals of the 21st century. Millions of people were prescribed potent opioids without being informed of their short- and long-term risks.
The cultural and prescribing context in the UK is different, and people tend to be prescribed less potent opioids in the first instance. However, hospital admissions due to opioid-related harms, have still doubled over a decade.
Using anonymised electronic health records from around two million people in the UK, our work at The University of Manchester found that prescribing in the UK for non-cancer pain increased between 2006 and 2017. During that period there was a five-fold increase in codeine prescriptions, a seven-fold increase in tramadol prescriptions, and a 30-fold increase in oxycodone prescriptions for non-cancer pain.
People with musculoskeletal conditions are particularly vulnerable to opioid-related harm due to factors including older age, being on drugs that suppress the immune system and medication for other pre-existing health conditions. Drug-interactions (when there is a reaction between two or more medicines leading to potentially more severe side effects) may be more common.
National bodies such as the National Institute for Health and Care Excellence (NICE), who publish guidance on the use of medicines, suggest opioids can be used infrequently for short-term pain relief in osteoarthritis. But they are no longer recommended for conditions such as fibromyalgia, as they were shown to be ineffective.
Long-term use
Given limited options for pain relief, it may be appropriate to take opioids in the short-term. But some people go on to use them long-term for a variety of reasons.
Long-term opioid use may be effective for some but can be associated with poor health outcomes including constipation, problems with concentration and cognition, increased risk of falls and fractures, and issues with breathing which can be life-threatening. There are emerging side effects to these drugs such as increased risk of infection, particularly concerning in people with musculoskeletal conditions who already have a lowered immune system. However, it is not currently possible to predict who may develop these side effcts before they get their prescription.
At The University of Manchester, some of our recent work shows that in the UK, in patients with fibromyalgia and rheumatoid arthritis newly starting on an opioid, up to one in three people transition to long-term use. For conditions such as axial spondylarthritis (an inflammatory arthritis that mainly affects the back), this was up to one in 3.5 to four people.
This means people with musculoskeletal conditions who are starting an opioid would greatly benefit from regular medication reviews in the community, proactive interventions to reduce pain without medications and early support to help manage pain.
The future
Opportunities such as new data sources, advances in methods and novel technology can allow important questions to be addressed that were not possible previously.
At The University of Manchester, Centre for Epidemiology Versus Arthritis, we are working on understanding how best to optimise these medicines. It includes:
- Identify risk-factors and groups of patients where harms outweigh benefits;
- Understand what prescribing factors (ie dose, type and patterns of use) lead to side effects important to patients;
- Develop better understanding of the association of opioids and emerging side effects such as risk of infection and effect on cognition;
- Predict individual risk of opioid-related harms, to help answer the question “what is my personalised risk of developing these serious side effects?”;
- Learn more about the benefits and harms of these drugs directly from patients by using digital data from smartphones;
- Implement research findings in real-time in clinical settings, before a patient receives their first opioid prescription to promote safe prescribing.
The aim is that people, along with healthcare professionals, can make more informed shared decisions to decide if these drugs are right for them.
Opioids and Me, by Louise Trewern

Six years ago, I went into my local community hospital for a rapid taper of high dose prescription opioids, due to my deteriorating health.
I had been on prescription opioids for over 12 years for pain due to fibromyalgia and osteoarthritis. As well as severe pain, I was sensitive to absolutely everything. I couldn’t even bear the cat walking across my lap. I assumed I was in so much pain because I needed another increase of drug dose; it never occurred to me that the pain medicines were not working. This only became clear after I was referred to the local Pain Rehabilitation Service.
Side effects
Over time I had started to display the side effects of long-term use of opioids. I developed opioid-induced hyperalgesia which meant I was extremely sensitive to pain. I had constant infections that required antibiotics, and often more than one course. I had repeated chest infections, sinus infections, skin infections and repeated vaginal and oral thrush. I developed quite severe sleep apnoea (when breathing stops and starts while you sleep) that was only picked up by an astute physiotherapist I was seeing about another problem. She referred me and I ended up with a full-face CPAP machine – this pumps air into a mask you wear over your mouth or nose while you sleep to improve breathing.
I could not tolerate any noise so the television had to be quiet, I couldn’t listen to music and too many people talking was painful. I would not answer the phone, even to family, and I became paranoid and depressed. As I never knew how I would be on the day, I wouldn’t accept invitations and eventually friends and family stopped asking. All of this also impacted my wife, who had become my full-time carer.
Sleep was another issue for me. The pain would wake me at night and I would not be able to drop off again. This resulted in me sleeping at odd times during the day and being awake half the night.
Between appointments at the pain clinic, I had two emergency admissions to hospital for opioid-induced impaction (where poo has built up in the rectum). Since starting on opioids, I was prescribed sachets of laxative to prevent constipation, a well-known side effect, but one Friday night out of the blue I just couldn’t go to the toilet. Over the weekend I had visits from an on-call GP, a district nurse who gave me enemas to help clear my bowel, and paramedics. Eventually on Monday morning an ambulance was called and I ended up in theatre. This happened twice in quick succession.
Positive change
The emergency admissions gave the criteria to get me into community hospital for a rapid taper. I went into the hospital a zombie, who didn’t want any noise and was sensitive to absolutely everything. At the time I was on several opioids including 320mg of oxycontin plus oxycodone liquid a day, with dihydrocodeine. I had diazepam for anxiety, and sertraline and duloxetine to help the pain. But I came out at the end of the week on 20mg of oxycontin, which I stopped over the course of the month. I was a completely different person.
Commitment
Going through withdrawal from opioids was no picnic. I was advised to gradually walk down the ward, as that could trigger endorphins, the body’s natural painkiller (something I had never heard before). I popped in my earphones and paced up and down constantly. It worked, so I carried on when I got home from hospital.
At first, I would take my wheelie walker to flat places like the seafront near where I live. As I got fitter, I was able to ditch the walker for walking poles and eventually no aids. I went into hospital weighing a dangerous 25 stone, and gradually I lost 8.5 stone by walking every day, eating properly and sleeping well for the first time in years.
With the combination of walking, eating well, connecting with nature, and learning self-management techniques, I came off all my multitude of opioids and drugs for pain.

I now no longer need the CPAP machine, and I am happier, healthier and fitter than I have ever been. Today I manage my pain by keeping as active as possible, walking, swimming in the sea year-round and using an exercise bike.
Inspiring others
I have now worked extensively with professionals and patients within the pain arena.
Learning about pain and how it works has been a linchpin for me to discover skills to self-manage my pain, and to help others go through the same process.
Useful resources
The British Pain Society, www.britishpainsociety.org
Flippin Pain public health campaign, www.flippinpain.co.uk
Footsteps Festival, www.footsteps-festival.co.uk
Live Well With Pain, www.livingwellpain.net
Pain Killers Don’t Exist, www.painkillersdontexist.com