From Manchester to Toronto – Improving lupus ‘brain fog’
In early 2021, Dr Michelle Barraclough, Research Associate for Manchester BRC’s Musculoskeletal theme, began a year-long research placement in Toronto to better understand ‘brain fog’ in lupus patients.
Here she shares her progress to date, and how this trans-Atlantic collaboration aims to improve care and treatments for patients.
For many people with systemic lupus erythematosus (SLE), cognitive dysfunction – which causes problems with a person’s memory and attention – can be a debilitating symptom that can make even the simplest mental tasks extremely difficult and tiring. The cause is incredibly complex with lots of factors affecting it, and likely to be different for each patient. This makes treatment decisions difficult and as such there are few effective treatments for it.
Based at the University Health Network’s (UHN) Toronto Western Hospital, Rheumatologist Dr Zahi Touma is a leading researcher in cognitive function in SLE and, alongside Dr Murray Urowitz and Dr Dafna Gladman, runs UHN’s long-established Toronto Lupus Research Programme. The plan to spend a year in Toronto researching cognitive dysfunction started in November 2019 during my annual work review with BRC Director Professor Ian Bruce. He was incredibly supportive and could see the benefits of a collaboration between Manchester and Toronto, and he kindly set up a meeting between myself and Dr Touma. After 20 months, many zoom meetings, late night grant writing, and navigating the Canadian visa system, I moved my family ‘across the pond’ to take up a Research Fellow post at UHN. This post was made possible, in part, thanks to a fellowship grant from The Arthritis Society.
Our ultimate goal is to learn more about cognitive dysfunction in SLE, so that we can eventually find better treatments that will improve cognitive function and quality of life for patients. I am incredibly lucky to have this opportunity and to join Dr Touma’s team for my year’s placement. Toronto’s research programme engages with over 2,000 lupus patients to collect valuable research data and work with patients to improve their care.
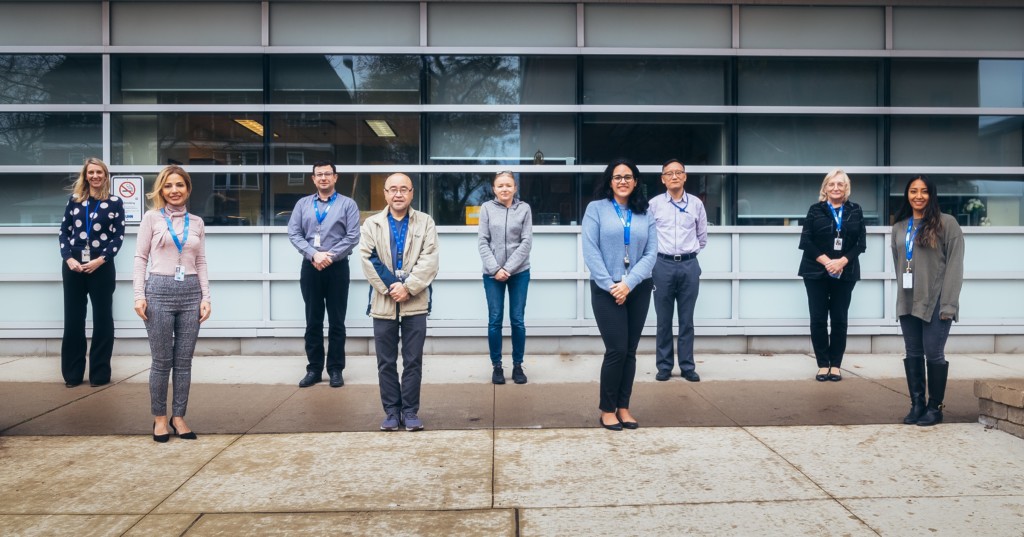
Some of Dr Touma’s Toronto research group (L-R): Dr Michelle Barraclough, Mahta Kakvan, Dr Zahi Touma, Michael Li, Joanna Kokalovski, Dennisse Bonilla, Jiandong Su, Anne MacKinnon, Janelle Lopez
Dr Touma has a large grant to work on a long-term study to phenotype (group) SLE patients based on their cognitive function. His multidisciplinary team also includes experts in neuropsychology, neurology, neuroimaging, psychiatry, immunology, epidemiology, and statisticians, which brings ideas from many perspectives to help in the battle against cognitive dysfunction in SLE.
Since joining Dr Touma’s team, some of the work I have been exposed to or directly involved in includes:
- Looking at differences between testing cognition in-person compared to remotely (online, with patients using their own computers). The hope is that these methods will both give similar results, which could eventually make it more convenient and accessible for patients.
- Looking for quicker, more accurate ways to measure cognitive problems in SLE. If a more universal tool, for example a set of computerised cognitive tests, could be established this could be easily used in clinics and help better understand individual patient problems.
- Defining and separating out cognitive fatigue, or ‘brain fog’, and cognitive dysfunction in SLE. Cognitive fatigue is more likely to be a feeling of struggling with concentration, memory, and daily tasks – still being able to complete things but maybe at a slower pace. Cognitive dysfunction is when these functions fail, an inability to remember, concentrate or complete daily tasks. These two issues are linked but it is not clear if fatigue always leads to dysfunction and how each can be treated.
- Using the large dataset we have here in Toronto to find potential drug treatments that might improve cognitive dysfunction in SLE. If links between medications and improved cognitive function can be found, then these medications can be tested in future clinical trials.

Toronto Western Hospital
Toronto is an amazing place with welcoming people from all over the world. The temperature is now dropping and I hope I’m ready for the cold winter! More importantly I hope to start recruiting to our functional Magnetic Resonance Imaging (fMRI) project (mentioned in my first blog) soon, which had to be delayed due to COVID-19 restrictions.
While this work was delayed, I have been able to work on other projects, including looking at some of the data from Dr Touma’s phenotyping study. This has been using machine learning techniques – statistical analysis using artificial intelligence (AI) – to group lupus study participants based on their individual clinical, psychological, and cognitive profiles. This important work helps us to better understand what treatments will be beneficial to individual patients with cognitive problems. This work has been presented at multiple conferences, including the American College of Rheumatology (ACR) Convergence (the leading rheumatology conference) and has won several prizes for best abstract. We have also been successful in obtaining an additional research grant, from Lupus Canada/Lupus Foundation of America to aid with this work and the future fMRI study.
When we do start the fMRI study, this will involve patients having a brain scan whilst undertaking cognitive tasks that test their memory and attention. We will be recruiting 20 patients with SLE and cognitive impairment, 20 patients with SLE but without cognitive impairment, and 20 healthy volunteers. I’m helping to link researchers from both the Toronto team and Professor Bruce’s team in Manchester. Participants will be recruited and tested in Toronto and analysis of the results will be completed both in Toronto and Manchester.
We believe that this study will highlight differences in how the brain works for people with lupus compared to those without. The belief is that the brain of people with lupus has to work harder than those without to maintain an adequate level of cognitive performance, which may lead to the feelings of ‘brain fog’ patients often describe in clinic. Brain fog is difficult to measure, which makes it difficult to test the effectiveness of potential treatments, but we hope this work will put us a step closer to finding treatment to help with cognitive dysfunction in SLE.
Toronto has been an amazing experience for me so far. I am developing as a researcher, learning from experts in multiple fields, generating many new ideas to further this research, and making plans for future collaborations. Most importantly though, this time away and this collaboration is strengthening our knowledge and understanding of cognitive dysfunction in SLE. This in turn is leading us closer to a treatment that will improve patient lives.
At the end of this placement, I will be bringing back to Manchester new knowledge, strengthened collaborations, future research plans, and a daughter with a very cute Canadian accent.
